Text Size
A
A
Reset Text
Questions? We're here for you.
Safety precautions related to COVID-19
Visiting Agrace:
If you have any questions before visiting Agrace, please call (800) 553-4289
The advice on this page was designed for Agrace’s hospice or supportive (palliative) care patients—and for their family members who are caring for them at home. The tips can help any person who has a serious illness. Touch or click the green menu above to jump to topics that interest you.
Families of Agrace Hospice Care patients should call us at (800) 553-4289 for advice, any time of day or night, if:
Agrace patients of their families may send non-urgent questions here:

Here’s what you can do to help manage symptoms that may be present in people with advanced illnesses. Click to learn more about any symptom that applies to you or your loved one.
How to improve breathing trouble (shortness of breath), a feeling of not getting enough air.
Tips to get relief from trouble "going to the bathroom," plus a printable bowel tracker.
Calming tips to try if a seriously ill person becomes restless, upset or tense.
Feeling uneasy or anxious is common during a serious illness; here's what you can do to help.
How to better prevent or control queasy feelings or vomiting due to a serious illness.
Ways to boost or conserve energy during times of feeling fatigue (lasting tiredness).
Care tips for calming and reassuring a person confused due to illness and/or medications.
Use our care guide and symptom tracker to help improve fluid build-up, shortness of breath, heart palpitations, fatigue and more.
These tips may help you care for people with Alzheimer's disease and other forms of dementia.
What should you know about giving medications to a loved one? Click the “+” to see details about each topic.
Here is our simple medication tracker. Print as many copies as you need to keep track of your medication doses and how you feel after taking the medication. This can help your care team know how well your medicines are working for you.
It is normal and expected to have some unwanted side effects when you take medications. You might notice side effects when you first start taking a medication, or if your dose needs to be increased or decreased.
If side effects of your medications are making you uncomfortable, talk to your health care provider or to your Agrace care team, if applicable. They will help you come up with a plan to get you feeling better.
Ask your primary doctor or hospice nurse before using this method, because some pills should not be crushed.
Allow time for the medicine to absorb. Do NOT swab or moisten the mouth for at least 30 minutes.
You may need to give “comfort medications” that are already in the home when a hospice patient is having trouble with symptoms such as:
These medications may include morphine, lorazepam, hyoscyamine and haloperidol. Here is a printable medication tracker and guide for how to give these medications.
Before you give any comfort medication to an Agrace Hospice Care patient for the first time, please call us at (800) 553-4289 and talk with a nurse to be sure it’s the right step.
Safely disposing of unneeded medications will prevent harm to children or pets who might take them accidentally—or to others who might take them illegally.
Ask your doctor or Agrace team to show you the best way to safely dispose of the kind of unused medication you have, especially if you have “controlled substances.” We may suggest steps like these methods:
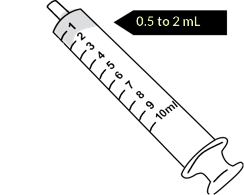
It is illegal to put needles and other sharp medical items in the trash, recycling or medication collection drop boxes.
If you use needles, syringes or lancets for medication administration, follow these steps to dispose of them properly:
More information can be found on the Wisconsin DHS site here, and on the Wisconsin DNR website: Managing household medical sharps | | Wisconsin DNR.
Pain Medication Side Effects
How can you help an ill person with their everyday care needs? Check the caregiver tips below, and ask Agrace if you would like more training on any of these topics.
Click the arrows to scroll left or right and see more topics.
How to avoid home safety hazards that could cause falls and painful injuries.
Learn steps to safely help a person rise, walk, shower and move from one position to another.
How to support a person who is eating and drinking less due to a life-limiting illness.
How to help a person who has limited mobility use a toilet, catheter, bedpan or incontinence supplies.
Follow these guidelines for using the medical equipment Agrace provides to our hospice patients.
Watch this video for help opening and using oxygen tanks.
Here are some of the questions family caregivers ask Agrace most often. Click the “+” for the answers.
For families of Agrace patients, our social workers can help you find resources in your community to support your needs. You can also explore these sources:
You may find these sites helpful if you are caring for a loved one with one of these life-altering illnesses:
Muscular Dystrophy Association
Wisconsin Dept of Health Services Support for People Dementia
Here are links to the full text of Agrace Hospice Care’s Patient & Family Care Handbook: In English In Spanish
Please copy a link and send it to your family members who live elsewhere, or anyone else who is going through a hospice experience and could benefit from knowing what to expect.
Caregiving is hard work. Watching your loved one decline is physically, emotionally and mentally draining. It is important to take time for yourself, to meet your needs.
The links below may help you, and your Agrace care team can provide support for you as you navigate this difficult and often emotional time.
The life changes and losses that may come with a life-limiting illness can have a lasting impact on people’s mental health and emotional and spiritual well-being.
The links below offer information that may help you. Agrace’s patients and their families can also turn to am Agrace social worker and spiritual & grief counselor for emotional support.
Do you need caregiving support beyond what you and your Agrace team can do? Finding and hiring extra help—or finding a place to live that offers caregiving—can be challenging. Many people do not know where to start.
Below are links that may help you with these tasks. You can also talk with an Agrace social worker for advice on these matters and any of the services listed here.
Hiring an agency is a personal decision and a business relationship between yourself/your family and care provider of your choice. Below are questions you may want to ask of the agencies you consider hiring:
Caring for someone with a life-limiting illness often raises complex questions about insurance, finances, legal matters and benefits. In addition to the state and national resources linked below, Agrace social workers can offer more guidance, information, and resources.
Agrace will pick up the durable medical equipment (DME) we supplied to our hospice patients (walkers, wheelchairs and hospital beds, etc.) when you no longer need it. If an item is yours to keep, your team will let you know. We cannot accept donations of other used medical equipment. Agrace may accept unopened packages of adult briefs (such as Depends®); please call your care team to pick them up.
Agrace thrift stores will take donated lift chairs that are clean and in good condition for resale.
To donate or recycle other equipment and supplies, please check these options:
Appetite changes are common in people with advanced illnesses. Many lose interest in eating. Sometimes, taste changes and favorite foods no longer taste good. People may say that their foods taste “off” or have a “metallic” taste.
People with serious illnesses may feel full or have no taste for food for many reasons, such as these:
It is natural and common for people to lose their desire to eat and drink as their condition declines. They may take only sips of liquids or small bites of food that can be swallowed easily. At some point, they may lose the ability to swallow well and may not take in anything at all.
A person who is not hungry or thirsty may feel discomfort from having a dry mouth. Using mouth swabs and moisturizers for the lips can help bring relief.
What can family or caregivers do to help?
The amount of urine a dying person produces typically decreases. Urine may become darker as both fluid intake and blood-flow through the kidneys decrease.
As the person declines, they may lose control of their bladder and bowels. This is completely normal. A urinary catheter or protective underwear may be needed to prevent skin breakdown and keep the person comfortable.
![]() Weakness and fatigue increase as death nears. The person may need help with simple tasks, such as taking a sip of water or turning in bed, and they may sleep most of the day.
Weakness and fatigue increase as death nears. The person may need help with simple tasks, such as taking a sip of water or turning in bed, and they may sleep most of the day.
For hospice patients, your team will help make a plan to ensure everyday needs, such as bathing and grooming, are met. We will offer suggestions for conserving energy, so time can be spent focusing on whatever the person enjoys. We work to help them be as awake as they would like and as comfortable as possible.
A person who is dying may have unusual breathing patterns and/or loud, wet-sounding breathing. Although these issues might be distressing to others, they rarely cause discomfort to the dying person.
Loud, rattling breathing may happen as the person become less able to swallow saliva or fluids. The “wet” sound is often due to a small amount of saliva in their throat that they are unable to cough up or clear. Suctioning has limited benefits, and it may make the congestion worse.
Family or caregivers can help by:
Breathing patterns may be slow and even at times and irregular and shallow at other times. Breaths may be separated by long pauses. These pauses are called “periods of apnea” and may last from seconds to more than a minute. As death nears, periods of apnea may become longer. A person may have periods of apnea for several days before death. Breathing may also be very fast at times.
Most people have an irregular pattern of breathing minutes before death. It is often followed by a short period of very shallow breaths, and then breathing stops.
If you question a hospice patient’s breathing comfort at any time, please call Agrace immediately.
Changes in blood flow may cause some noticeable changes in the person’s body. Hands and feet may become darker or paler and colder to the touch. The skin on the arms and legs may appear blotchy and purplish. This discoloration, called “mottling,” is the result of reduced blood flow. An increase in mottling can be a sign that death may be near. People who are dying are not usually aware of these changes and rarely feel discomfort from them.
Some people develop a fever as they near death. Medication may be given for the fever, but it does not always work to reduce the temperature. Most people do not appear uncomfortable because of fever.
![]() Managing pain is an essential part of end-of-life care. Pain can almost always be controlled, and the person can be kept comfortable through the dying process. Medications can be used to keep them comfortable without too many side effects and without excessive drowsiness.
Managing pain is an essential part of end-of-life care. Pain can almost always be controlled, and the person can be kept comfortable through the dying process. Medications can be used to keep them comfortable without too many side effects and without excessive drowsiness.
Please talk with your Agrace team if you have any concerns about managing pain for a hospice patient.
![]() As death approaches, it is common to feel fear and anxiety about the dying process and death itself. The person who is dying may show their anxiety through anger, withdrawal, restlessness, demanding behavior, irritability or crying.
As death approaches, it is common to feel fear and anxiety about the dying process and death itself. The person who is dying may show their anxiety through anger, withdrawal, restlessness, demanding behavior, irritability or crying.
Most people feel some level of anxiety at times. Some ways to ease anxiety include comforting them with understanding, touch, active listening, calmness and medication.
It may also help to keep lights low, keep the room quiet or play soothing music, and try relaxation techniques such as deep, controlled breathing.
Some people become minimally responsive for hours or even days before death. They show little awareness of their surroundings. Others remain clear and alert up to the last few moments. Generally, people are gradually less and less alert as death approaches.
As a person becomes less responsive, there may be less opportunity to have meaningful communication. Even if they cannot respond, they may continue to hear and have a level of awareness.
You should always assume the person hears everything you are saying. Talk to them as clearly and directly as if they were awake and alert.
![]() Some people have a period of restlessness as death approaches. Restlessness may be caused by physical, emotional or spiritual factors. You may see them picking at their clothes or bedding, reaching into the air or moving about in bed. It can help if you provide a calm and reassuring environment.
Some people have a period of restlessness as death approaches. Restlessness may be caused by physical, emotional or spiritual factors. You may see them picking at their clothes or bedding, reaching into the air or moving about in bed. It can help if you provide a calm and reassuring environment.
If restlessness appears to be bothersome for a hospice patient, contact your Agrace team for suggestions.
Sometimes a person who is nearing death will use words and phrases that lead others to believe they are confused. This language can be very meaningful to the patient and their family, and it can be symbolic of the life they led.
People who are dying may talk about events in their past. They may use words that describe the need to move, travel or go to another place, or they may talk about a specific time that they will die. They may speak to someone who is no longer alive or express a need for reconciliation or forgiveness. This is common at the end of life.
Offer your supportive presence and pay attention to what is said. It is often very meaningful. Many dying people do not appear to be distressed because of symbolic language or visions.
If you are with a hospice patient who seems distressed or you have concerns about any end-of-life matter, contact your Agrace Hospice Care team.
People often become less interactive and more withdrawn as death nears. This may be partly due to physical factors but may also reflect the person’s need to process the situation emotionally and/or spiritually.
Withdrawal can be a difficult experience for loved ones. A loving, supportive presence may be all the person needs or wants at this time.
To compliment a staff member, please email Agrace’s Patient and Family Relations Team.
Call to talk to an interpreter / Tenemos intérpretes disponibles: (800) 930-2770
©2024 Agrace - All Rights Reserved. | Privacy Policy
